The VCI score is a new and simple communication tool to describe tracheal intubation using videolaryngoscopy. It encompasses three critical components thought to be relevant to videolaryngoscopy use:
- Generic blade shape
- Glottic view at the point of tracheal intubation or attempted intubation using POGO
- Ease of tracheal tube delivery
The first element of the score considers the type of videolaryngoscopy blade used. The ‘M’ refers to a Macintosh-shaped blade, ‘H’ for a hyperangulated blade and ‘S’ for a straight shaped laryngoscope blade.
The second component describes the percentage of glottic opening (POGO) visible to the nearest quartile at the time of intubation. This is a crucial nuance since the glottic view, which allows successful tracheal intubation to be achieved, may not necessarily be the initial or best view obtained.
The last part of the score describes tracheal tube delivery and is detailed by one of the following qualitative terms: Easy (‘E’), Difficult (‘D’), or Failed (‘F’). While subjective, the following provides a pragmatic guide:
- Easy: straightforward first-time intubation of the trachea (minor adjustments to rotate the tube to avoid the arytenoids and hold up are acceptable. For hyperangulated blades, the use of a stylet is part of the technique and does not constitute an airway adjunct). Channel should be specified if the channel was used for tube delivery when using channelled blades.
- Difficult: Everything between the two extremes of Easy and Failed and indicates that tube delivery was not straightforward and something ‘else’ had to be done to enable passage of the tube such as manipulation of the tracheal tube with additional equipment (e.g. change from a stylet to a bougie or vice versa). A free-text comment must be provided highlighting any difficulties.
- Failed: Inability to intubate the trachea despite the use of adjuncts. Again comments highlighting the reason for failure should be provided.
The resulting score has three parts. For example, M75E would represent tracheal intubation using a Macintosh-shaped videolaryngoscopy blade with a 75% glottic opening at the time of tracheal intubation, which was uncomplicated.
The airway grade H50D (flexible scope) would represent tracheal intubation using a hyperangulated blade with 50% glottic opening at the time of tracheal intubation. Additionally, a flexible scope was required to enable passage of the tracheal tube.
To think about why we might need the VCI score, we should first consider why we communicate and document anything at all about tracheal intubation. Firstly, we all know that it is best practice is to keep a clear and accurate medical notes of the care we provide to patients. Secondly, knowledge of how tracheal intubation was previously achieved is useful in planning and preparing for subsequent airway management of that patient. And finally, for medicolegal purposes our documentation needs to be easily interpreted retrospectively to paint a precise picture of what we did.
The VCI score is a method to succinctly communicate airway management using videolaryngoscopy. Various other methods exist but do not consider the type of blade or the difficulty of tube delivery and are not used universally. This service evaluation aims to understand how the VCI score performs at a practical level in diverse settings.
The shape of the videolaryngoscope blade is one of the most critical determinants of the technique used to obtain a view of the glottis. At present, blade shape falls mainly into one of two categories for adults: a Macintosh-shaped blade or a hyperangulated blade. In paediatrics, a straight blade is also commonly used.
By focussing on generic blade shape, we can make educated deductions about how the glottic view was obtained and removes the need to be familiar with all videolaryngoscopy devices available.
The POGO score represents the percentage of glottic opening seen, defined by the linear span from the anterior commissure to the inter-arytenoid notch. The POGO score has been extensively validated in the literature and demonstrated high inter-rater reliability. Subdividing glottic opening into quarters is intuitive, simple and easily communicated. The descriptive nature of these POGO scores is readily understood with minimal explanation and does not require any additional knowledge of anatomy other than the view of the vocal cords. Furthermore, using POGO scores may also have the advantage of allowing disease progression in Head and Neck pathology to be recorded where the POGO score may have changed with subsequent tracheal intubations. Decreasing POGO with serial/subsequent intubation may be concerning and you may see this impact in the third part of the VCI score (or lead to a change of blade or technique completely).
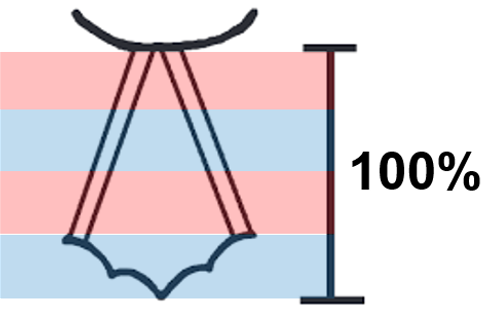
Videolaryngoscopes often allow the glottic inlet to be easily visualised, yet tracheal tube delivery through the vocal cords may remain challenging (the frustrating ‘good view, can’t intubate’ scenario). Recording POGO at the moment of intubation attempt is important since the glottic view at which successful tracheal intubation using videolaryngoscopy is achieved may not be the same as the initial or best view obtained. Recording this allows the reproducibility of the tracheal intubation experience and documentation to be as accurate as possible.
Using the Cormack-Lehane score is unhelpful to describe tracheal intubation using videolaryngoscopy since it describes the glottic view achieved by aligning the oral, pharyngeal and laryngeal axes. Direct laryngoscopy aims to obtain the best view possible since this should allow the most straightforward passage of the tracheal tube. Whilst not a perfect score to describe direct laryngoscopy, the Cormack-Lehane score has been widely accepted probably because increasing Cormack Lehane grades correlate well with increasing difficulty with tracheal intubation. Videolaryngoscopes have a camera positioned in the distal third of the blade which means that obtaining the glottic view is usually straightforward since the view point is already beyond most of the anatomy (if not all!) that would have obstructed the view with a direct laryngoscopy technique. Furthermore, videolaryngoscopy techniques do not require the three axes to be aligned. For these reasons, unlike with direct laryngoscopy, the ease at which the glottis can be viewed may not necessarily correlate with the ease of tracheal intubation.
A score describing tracheal intubation using videolaryngoscopy would be incomplete without some comment about tube delivery because of the well recognised phenomenon of ‘good view, can’t intubate’. The tube delivery part of the score should not be confused as describing the overall tracheal intubation process. This component of the score is simply describing the tube delivery and may be classified as Easy (E), Difficult (D) or Failed (F). Using these descriptors to communicate the ease of tracheal tube passage allows critical information about the technique to be comprehensively communicated. If a ‘D’ or ‘F’ is noted then further information should be provided or sought.
No! However, none of the currently available scores are perfect. We are hoping by assessing the usability and reproducibility of the VCI score on a much wider scale in the VCI Project, we will be able to demonstrate what we think are the strengths of the VCI score – it can be applied to any videolaryngoscope device, it is simple to use and interpret and communicates succinctly the practically useful key elements of tracheal intubation using videolaryngoscopy. Furthermore, a code D or F for tube delivery serves as a rapid alert to search for more information.
Yes. Our pilot study investigated whether two anaesthetists could generate concordant VCI scores in real-time for a given patient undergoing elective airway surgery. We found that two anaesthetists produced identical VCI scores in 34 out of 35 patients. The VCI project aims to assess the usability and reproducibility of the VCI score more rigorously in various patient groups and clinical settings.
The VCI score is intended for any healthcare professional who is involved in airway management, for those who perform or assist with tracheal intubation and those who look after intubated patients.
